A New Quality of Care Framework to Measure and Respond to People’s Experience with Self-Care
To mark International Self-Care Day, Population Services International and partners under the Self-Care Trailblazers Working Group are sharing a new Quality of Care Framework for Self-Care to help health systems monitor and support clients accessing health care on their own—without hindering clients’ ability to do so. Adapted from the Bruce-Jain family planning quality of care framework, the Quality of Care for Self-Care includes five domains and 41 standards that can be applied to a broad range of primary health care approaches to self-care.
July 24th marks International Self-Care Day, reminding us that to strive for universal health coverage, it is vital to adopt approaches that support individuals as active participants and decision-makers in their own health care.
While the landscape for self-care is broad, incorporating health literacy and physical and mental well-being, there is growing interest in self-care interventions or self-care approaches that see information, products, and services previously “controlled” by a provider, typically in a health facility, evolve so that people can play a greater role in managing their health care. Such self-care interventions are evidence-based health actions (often hinging on high-quality drugs, devices, diagnostics, and/or digital products) that can be provided fully or partially outside of formal health services and can be used with or without the direct supervision of health care personnel. Examples include self-injectable contraception, diet and lifestyle adjustments for heartburn relief in pregnancy, human papillomavirus (HPV) self-sampling, or HIV self-testing.
This trend is a result of a broad range of forces, not least, advances in the fields of medical and digital technologies. The COVID-19 pandemic also places an unprecedented spotlight on individuals self-managing health needs and on governments actively seeking help from individuals, communities, and national and international health systems in their efforts to combat the pandemic.
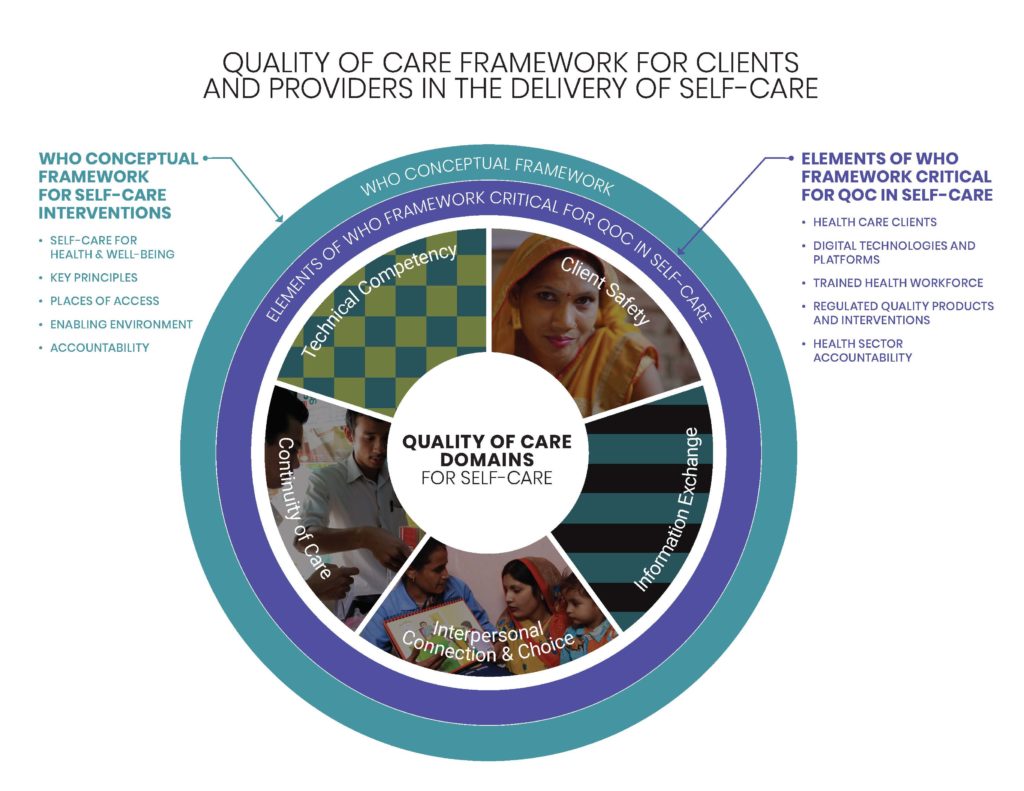
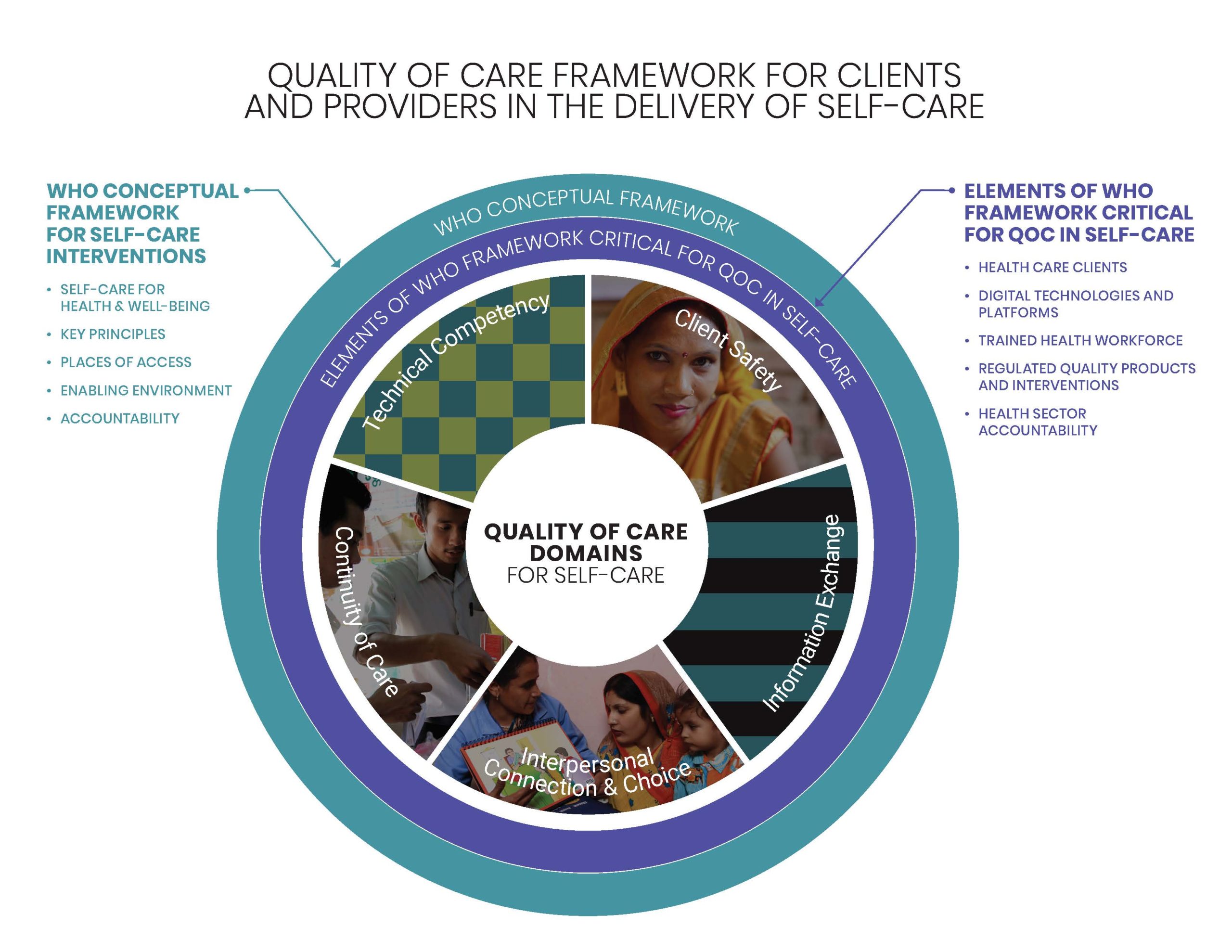
Population Services International (PSI) and a consortium of organizations under the auspices of the Self-Care Trailblazers Working Group have developed a Quality of Care Framework for Self-care aligned with the WHO Consolidated Guideline on Self-Care Interventions for Health. The WHO put forward that it is possible to think about self-care from two complementary perspectives: one focused on improving the capacity of individuals to self-manage their care and another focused on reorienting the health system so that, as people become more engaged in their health, the health system is there to meet them.
How Was the Framework Developed?
In 2018-19, the Support for International Family Planning and Health Organizations (SIFPO) 2: Sustainable Networks project, funded by the U.S. Agency for International Development (USAID), was supporting several self-care interventions, including contraceptive self-injection and HPV self-sampling. Recognizing the gap in linking quality of care for these interventions to each other and to health systems, staff began to work with the Self-Care Trailblazers Group to organize quality of care in self-care more broadly.
A driving question for this group was, “If someone engages in self-care—on their own time and often in a private setting—how can quality of care be ensured?” Any health system has at a minimum a standard of duty to ensure quality, but what happens when the health action takes place outside the confines of a facility, or sometimes outside of any health care interaction at all? How should the health system monitor and support the care a client is accessing on their own while ensuring its approach does not inadvertently hinder a person’s ability to manage their own care? Meanwhile, what quality of care approaches already exist into which the needs of self-care can be woven?
With these questions in mind, the globally accepted Bruce-Jain Quality of Care Framework’s domains were reviewed, proposed, and adapted as core components for monitoring the quality of care in any self-care intervention, and not limited to family planning. While quality of care has been monitored in family planning service delivery under these domains since the Bruce-Jain framework was published in 1990, the Quality of Care Framework for Self-care goes beyond evaluating provider and facility quality of care and moves the focus to elements critical for quality of care specific to self-care: health care clients, digital technologies and platforms, regulated quality products and interventions, the trained health workforce, and health sector accountability.
These elements were selected from the WHO Conceptual Framework for Self-Care Interventions. While all elements in the WHO framework are critical for the ecosystem that enables self-care—for example, psychosocial support and economic empowerment—the selected elements for this quality of care framework are specifically valuable for monitoring and supporting quality when clients are engaging with self-care on their own, or in partnership with a health care provider.
What is In the Quality of Care Framework for Self-care?
The five domains that sit at the core of the framework are:
- Technical competency
- Client safety
- Information exchange
- Interpersonal connection and choice (to engage in self-care)
- Continuity of care
Though grounded in family planning, these domains and the framework may be applicable to a broader range of primary health care approaches to self-care. Within these five domains, a total of 41 standards comprise the framework and each can be adapted for any self-care intervention.
Instead of primarily assessing a provider’s technical competency to provide quality health care, standards in the self-care framework evaluate a client’s capacity to manage their own care with safety and competency:
- Client can accurately determine if they are experiencing a side effect or complication.
- Client demonstrates the knowledge and skills needed to competently self-manage care (e.g., through self-screening, self-testing, self-referral, etc.).
Standards also evaluate health care provider/worker roles in a new way, by assessing their capacity to support people-centered self-care, whether offered directly or with a digital application taking their place at times:
- Health provider/worker or digital application gives information regarding benefits, risks, and side effects of a chosen service prior to receipt.
- Health provider/worker or digital application provides information or care in a respectful, empathetic, non-judgmental way that is free from coercion and facilitates the client’s agency.
Respectful and dignified care is given a strong emphasis throughout the domains of Interpersonal Connection and Choice and Information Exchange. While these components have long been a part of high-quality, empathetic care that builds individuals’ self-reliance, the self-care framework gives us a new opportunity to highlight these people-centered aspects of care, responding to what recent evidence demonstrates is a priority for many. Standards include:
- Client’s experience of care during all self-care interactions is dignified, empathetic, and respectful.
- Client accesses care or information that does not vary in quality because of their personal characteristics such as age, marital status, gender, disability, ethnicity, geographic location, and socioeconomic status.
Importantly, several standards acknowledge that the health sector has a role to play in monitoring quality and the client experience:
- There is a mechanism to assess if a client can access comprehensible information that is responsive to their expressed needs and includes information regarding benefits, risks, and side effects.
Who Should Use the Framework?
The Quality of Care Framework for Self-care is intended for:
- Implementers who wish to ensure people-centered quality of care via any type of self-care intervention(s)
- Ministries of Health who are accountable for ensuring quality of care in self-care across the health system, in both the public and private sectors
- Policymakers/investors/donors/researchers who wish to verify that a self-care intervention applies best practices in people-centered quality of care
How Can the Framework be Implemented and Measured?
The Quality of Care Framework for Self-care is intended to complement existing quality of care frameworks. It can help an implementing partner or a Ministry of Health to augment a current quality of care system for self-care, or to integrate various self-care interventions more effectively and efficiently with each other. Alternatively, it can be applied to strengthen the quality of care features that an individual self-care intervention might require of the health system.
Perhaps, and of critical importance for meeting an individual’s unique self-care needs and preferences, this framework will allow programmers, researchers, and policy makers to measure the quality of an individual’s experience with self-care more effectively—and then make responsive changes. If we can no longer observe a provider-client interaction as a way to determine if quality standards were adhered to, we must find creative solutions for monitoring, evaluating, and responding to quality of care.
To this end, it is essential to find a way to ask individuals how they valued their experience, if they were satisfied with their health outcomes, and if they have confidence in the health system. As the Lancet Global Health Commission acknowledged, measurement is key to accountability and improvement, and measures must reflect what matters most to people. Holding the client experience at the heart of any approach may be what matters most to the delivery of high-quality self-care.
What’s Next for Quality of Care in Self-care?
A growing number of initiatives are advancing self-care, examining the evidence and possible best practices for its growth and development, including the USAID award Research for Scalable Solutions (R4S), led by FHI 360 and partners. Innovations abound and are going to scale, whether through the use of Artificial Intelligence to support self-diagnosis and self-management or the advancement of initiatives such as Patient Activation Measures (PAM), which support health care provider decision-making by measuring an individual’s knowledge, skill, and confidence in managing their own health care.
This Quality of Care Framework for Self-care will be further discussed and fine-tuned in international forums in the following quarter, to be published before the end of year and potentially integrated with implementation guidelines in 2021. Promoting a more holistic and integrated approach to quality of care for self-care will help individuals, communities, and entire health systems enhance self-care’s contribution to navigating the new world we find ourselves in today—and the health care we want for tomorrow.