Recap of “Connecting Conversations” Series: Learning from Our Mistakes

On August 26, Knowledge SUCCESS and FP2020 hosted the fourth session in our new webinar series, “Connecting Conversations”—a series of discussions on adolescent and youth reproductive health. Missed this webinar? You can follow the links below to watch the recording and register for the fifth session in the first module.
Note: The French recording will be available within the next week.
Note : L’enregistrement français sera disponible dans la semaine prochaine.
Overview: Learning from Our Mistakes
The fourth webinar in our “Connecting Conversations” series discussed the value of acknowledging missteps and learning from them to adapt and improve our work. Featuring three experts—Dr. Venkatraman Chandra-Mouli (Scientist, Adolescent Sexual & Reproductive Health, Department of Sexual and Reproductive Health & Research, WHO), Ms. Bless-me Ajani (Project Lead, Global Girls Hub Initiative), and Dr. Sonja Caffe, (Regional Adolescent Health Advisor, PAHO/WHO)—the session built on themes from the first, second, and third sessions in the series.
Dr. Venkatraman Chandra-Mouli provided an overview of the topic. Last year, to commemorate the 25th anniversary of the International Conference on Population and Development, WHO and UNFPA brought together stakeholders to reflect on 25 years of lessons learned—from successes to failures. These insights were published in a supplement to the Journal of Adolescent Health. Chandra-Mouli stressed that this work, and this presentation, is not about blaming any individual or group. This is about acknowledging our shortfalls, learning, and avoiding them in future programs. He presented the five main types of problems seen across adolescent and youth reproductive health.
Problem #1: One Size Fits All
While there is widespread recognition that adolescents are a heterogeneous group, most programs still take a one-size-fits-all view. We need to use a tailored approach to respond to different segments of the adolescent and youth population —regardless of marital status, gender, school attendance, and whether they are parents or not.
Problem #2: Poor Reach
Many adolescents are not reached by intended interventions. We must assess whether we are reaching who we intended to reach. If not, we must adapt our delivery strategies accordingly.
Problem #3: Inadequate Fidelity
Effective interventions tend to be implemented without adequate attention to the factors that make the program effective—thus, they are often no longer effective. Each intervention needs to be delivered as it was designed.
Problem #4: Low Dosage
Interventions delivered using only one channel, or limited sessions, do not work. Programs intended to improve knowledge, attitudes, beliefs, and behaviors should be delivered with intensity and sustained over time.
Problem #5: Inappropriate Use of Training
Our programs often over-rely on training. Training is often the only approach used to approve health workers’ attitudes, competencies, and motivation. It is often done poorly and without crucial participatory elements. We need to implement a package of proven approaches to motivate and enable health workers to do their best—including supportive supervision, collaborative peer-to-peer support, good working conditions, and better infrastructure.
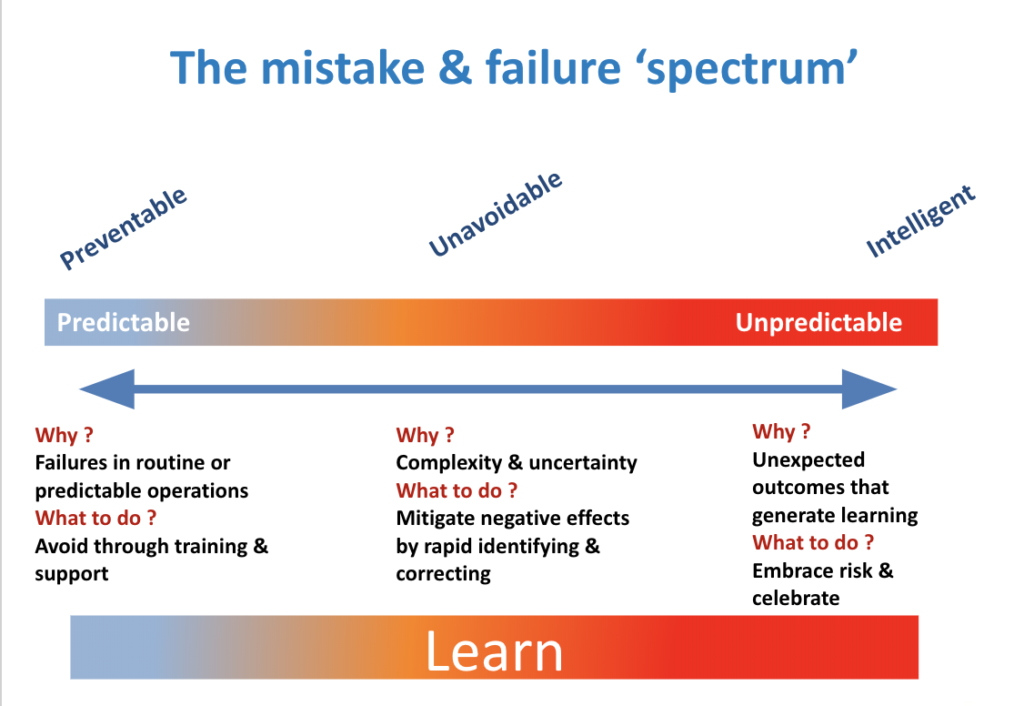
Chandra-Mouli wrapped up his presentation by emphasizing that “there is a deathly silence about mistake and failures.” We need to openly discuss our mistakes—and those of others—as we learn from success. He presented the mistake and failure spectrum graphic (see below), developed by Clea Finkle of The Bill & Melinda Gates Foundation—which includes preventable, unavoidable, and intelligent mistakes. We must minimize avoidable mistakes, mitigate unavoidable ones, and accept that innovation and risk go hand-in-hand. Embracing risk and failure, we can learn from all three kinds of mistakes. Only when we do this can we plan more effective programs.
Connections among Panelists’ Experiences
The majority of the session was dedicated to a conversation among the experts, moderated by Emily Sullivan, Adolescent and Youth Engagement Manager at FP2020. The panelists discussed their work and how they have learned from past mistakes. To start this conversation, Sonja Caffe and Bless-me Ajani both commented on Chandra-Mouli’s presentation.
Dr. Sonja Caffe shared perspectives from the Latin America and Caribbean (LAC) region. She named two reasons why people may be hesitant to openly share their mistakes. For one, people often put their heart and soul into the work. It can therefore be difficult to admit when something isn’t generating results. We still need to advocate for adolescent health, but we also need to adapt based on evidence. Second, many organizations are afraid to admit to failure out of fear that they will lose donor funding. Once we all recognize that learning from mistakes promotes growth, we can open up space to strengthen monitoring and evaluation and make sure we are constantly improving.
Bless-me Ajani responded with some overall comments: Regarding the overuse of training, she mentioned the importance of addressing health workers’ attitudes and behavior. They have technical knowledge, but we also need to engage with them to address stigma and encourage adolescent-responsive health care. In talking about mistakes, it is also important to include donors as part of these conversations so they can support the integration of learnings into scale-up. We cannot expect broad, national change from one-off programs.
Questions from Participants
How do we prevent getting stuck in a cycle of one training after another, without seeing broad changes?
Caffe said that we are in this cycle because of habit—we cover a certain number of modules or topics, without understanding how learning really works. PAHO is now thinking about adult learning in a different way. Every health worker comes to the table with some knowledge and experience—how do we maximize their learning and change the paradigm? We need to allow people to learn from each other, rather than a top-down trainer model. Horizontal learning, and learning from experience, is more effective.
Chandra-Mouli added that training is important, but we know that training is best done in small groups with focused topics, using multiple methods. If we do training, we need to do it well and ensure we carefully match it with the competencies we are trying to improve.
Training must also be combined with other interventions. There are a number of proven approaches to improve competencies among health workers. For example, we can provide health workers with reference materials to help reinforce their training. Another huge factor is motivation. Health workers may know what to do in theory, but they may not do it because their beliefs or attitudes may be preventing them—for example, if they believe that providing contraception to adolescents is wrong. These issues cannot be addressed through training alone. We need to challenge their attitudes and behaviors—this can be done through collaborative learning and on-the-job training.
How Can Governments, Donors, and Others Ensure Accountability?
Caffe began by discussing the importance of incentives for health workers’ improvement. Governments should have a continuing dialogue with health workers to understand what motivates them to improve their quality. This goes beyond financial incentives to include recognition, acknowledgement, and career advancement.
Chandra-Mouli mentioned ways to increase accountability at the local level—including checklists, scorecards, public hearings, and audits. At the national level, we can think more broadly. For example, in 2014, India launched a large adolescent health program. Two years in, the government recognized it was not going as well as they’d hoped. They worked with WHO to do a review in four states and at the national level. Government leaders accepted the constructive criticism from WHO and other stakeholders, because it was a safe space and they had an overall commitment to improve. We need to create and encourage a collaborative, trusting environment to talk about mistakes. We don’t want to celebrate avoidable failures—for example, if a program does not do a situation analysis and the program failed. However, if a program makes mistakes while doing the best they can, and learns from these mistakes, this should be celebrated.
Ajani agreed that governments need to find ways to motivate health workers, and not necessarily with money. Governments need to offer ways for health workers to advance in their career paths, based on performance and competencies in adolescent reproductive health. Governments also need to coordinate training—so partners are not training the same participants—in order to maximize resources.
Chandra-Mouli added that, while we need to hold health workers accountable, we also need to celebrate their work and recognize the challenges they face. Health workers need to be paid on time, they need to be treated fairly, and they need protective equipment so they can be safe and provide good quality care. We need to create a chain of accountability: Before holding health workers accountable, we need to ensure that governments protect and support health workers.
How Can We Overcome Low-Dose, Low-Duration Programs and Ensure that Programs Have Higher Fidelity to Evidence?
Caffe mentioned an evidence-based program in the LAC region, which reaches over 200,000 families a year across in several countries. After several years of implementation, many staff were altering the program—for example, shortening the length or number of sessions. Caffe stressed that programs can adapt to the local context, but it’s important to avoid changing the core elements of a program. Otherwise, it’s not the same program. PAHO developed tools to re-emphasize the importance of the core program, and explained that adaptation has to be within the core structure. They listed things they couldn’t change, and introduced these materials to country implementers. This improved the program quality and challenged the team to get the results they desired by following the program more faithfully.
Chandra-Mouli added that the focus needs to be on implementation and measurement. We can learn from the private sector and the pharmaceutical field to use management to improve performance. COVID-19 has shown that this doesn’t require a lot of funding. Low-income countries have shown that they can do program management very well.
Ajani added that this is an important opportunity for collaboration. We can’t implement programs piecemeal. Peer education, for example, can be a fantastic approach (including positive impacts on the peer educators themselves), but we are often not implementing this strategy in combination with others that enable the social support necessary for sustained behavior change among young people to compliment the peer education.
Chandra-Mouli reiterated that we need a safe and supportive environment for young people. We need a package of interventions, not one on its own. He also stressed that we need to locally adapt programs and to test them in various contexts. But once we test and demonstrate that a program is feasible, acceptable, and effective, we need to maintain consistency in order to see results.
What is the Evidence for the Effectiveness of Peer Education?
Chandra-Mouli explained that we have clear recognition that young people look to each other for tools and information. Evidence shows that peer education programs, when well-designed and well-conducted, can improve knowledge and improve attitudes—however, there is limited evidence on their impact on behavior change. This is not a problem, so long as we acknowledge the limits of peer education, along with the benefits—including building community, creating empathy, and fostering ownership. We should continue doing peer education well, and make sure it is combined with other interventions. It is also important to meaningfully engage young people in program design, implementation, evaluation, and accountability.
When Do We Bring Young People into the Conversation?
Chandra-Mouli answered that the WHO engages youth in all substantive work they do. They select them objectively, support them to make their contributions, acknowledge their contributions, and pay them for their participation.
Ajani stressed that we need to involve young people from the beginning—specifically, in writing proposals for interventions, designing programs, and making policies. She also stressed the need to align our projects with government priorities so these projects can be sustained by governments after the project ends. Young people should also be involved in the development of policies that affect them.
Closing Remarks
To sum up the session, Caffe reflected: “Mistakes might be painful, but when we transform them into lessons learned, we are strengthening the adolescent health field…. We need to celebrate lessons learned and mistakes, because that’s how we will move forward.”
Sullivan ended by acknowledging Anand Sinha’s work on failure, and encouraged participants to work together to create a culture of acknowledging mistakes and failures, ultimately leading to stronger programs.

Selected tools and resources mentioned during the session:
- GAGE Rigorous Review: Girls’ clubs, life skills programmes and girls’ well-being outcomes
- TARUNYA project evaluation
- Journal of Adolescent Health supplement
- What Does Not Work in Adolescent Sexual and Reproductive Health: A Review of Evidence on Interventions Commonly Accepted as Best Practices
- We Need to Talk About Failure
- Looking Back and Moving Forward: Can we accelerate progress on adolescent pregnancy in the Americas?
Missed this Session? Watch the Recording!
You can watch the webinar recording (available in both English and French).
About “Connecting Conversations”
“Connecting Conversations” is a series of discussions on adolescent and youth reproductive health—hosted by FP2020 and Knowledge SUCCESS. Over the next year, we will be co-hosting these sessions every two weeks or so on a variety of topics. You may be thinking, “another webinar?” Don’t worry—this is not a traditional webinar series! We’re using a more conversational style, encouraging open dialogue and allowing plenty of time for questions. We guarantee you will be coming back for more!
The series will be divided into five modules. Our first module, which started on July 15 and runs through September 9, is focusing on a foundational understanding of adolescent development and health. Presenters—including experts from organizations such as the World Health Organization, Johns Hopkins University, and Georgetown University—are offering a framework for understanding adolescent and youth reproductive health, and implementing stronger programs with and for young people. Subsequent modules will touch on themes of improving young people’s knowledge and skills, providing family planning and reproductive health care, creating supportive environments, and addressing the diversity of young people.




