Tag:
service delivery

Knowledge SUCCESS interviewed global health professionals on progress made since the 1994 ICPD Cairo Conference. The first in a three-part series features Mary Beth Powers, President and CEO of the Catholic Medical Mission Board.

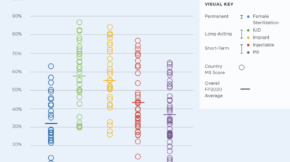
The Research for Scalable Solutions and SMART-HIPs projects—hosted a four-part webinar series on Advancing Measurement of High Impact Practices (HIPs) in Family Planning. The webinar series aimed to share new insights and tools that can strengthen how HIP implementation is measured in order to support strategic decision-making.

Gain insights on the vital role of Senegal's self-care guidelines and their impact on reproductive health goals. And, delve into the intersection of knowledge management and self-care guidelines, showcasing the collaborative efforts between Senegal and Knowledge SUCCESS.

Obtenez des perspectives sur le rôle essentiel des directives d'auto-soins du Sénégal et leur impact sur les objectifs de santé reproductive. Plongez également dans l'intersection entre la gestion des connaissances et les directives d'auto-soins, mettant en lumière les efforts collaboratifs entre le Sénégal et Knowledge SUCCESS.

Knowledge SUCCESS’ Brittany Goetsch chatted recently with Dr. Mohammad Mosiur Rahman, Professor, Department of Population Science and Human Resource Development, University of Rajshahit, the principal investigator (PI) of the research team, to learn how they used secondary data sources to explore the similarities and differences in facility readiness to provide FP services across 10 countries.

La 10e Réunion Annuelle du Partenariat de Ouagadougou (RAPO) a été placée sous le thème : «Planification Familiale en contexte de crise humanitaire : Préparation, Réponse et Résilience ». La communauté du Partenariat est consciente de l’urgence d’agir, étant donné les répercussions de ces crises sur les droits et les besoins essentiels des communautés. La question des crises humanitaires et leur impact sur la planification familiale mérite d’être davantage au cœur des discussions.

On April 27, Knowledge SUCCESS hosted a webinar, “COVID-19 and Adolescent and Youth Sexual and Reproductive Health (AYSRH): Stories of Resilience and Lessons Learned from Program Adaptations.” Five speakers from around the world presented data and their experiences on the impact of COVID-19 on AYSRH outcomes, services, and programs.

Safe Delivery Safe Mother aims to address high fertility and reduce maternal mortality in Pakistan. Recently, the group implemented a pilot project that trained over 160 government-deployed Skilled Birth Attendants (SBAs) in the Multan district of the Punjab province. The six-month pilot project concluded in February. The Safe Delivery Safe Mother team is in the process of sharing recommendations on how to increase the use and acceptance of post-partum family planning with the Pakistani government and other partners.

Increasing investments in emerging technologies across low- and-middle income countries have created unprecedented opportunities to leverage digital innovations to enhance voluntary family planning programs. In particular, the use of artificial intelligence (AI) to gain new insights into family planning and optimize decision-making can have a lasting impact on programs, services, and users. Current advances in AI are just the beginning. As these approaches and tools are refined, practitioners should not miss the opportunity to apply AI to expand the reach of family planning programs and strengthen their impact.
In July 2021, USAID’s Research for Scalable Solutions (R4S) project, led by FHI 360, released the Drug Shop Operators' Provision of Injectable Contraception manual. The handbook shows how drug shop operators can coordinate with the public health system to safely provide an expanded method mix that includes injectables, as well as training for clients on self-injection. The handbook was developed in Uganda in partnership with the National Drug Shop Task Team but can be adapted to various contexts in Sub-Saharan Africa and Asia. Knowledge SUCCESS’ contibuting writer Brian Mutebi talked to Fredrick Mubiru, Family Planning Technical Advisor at FHI 360 and one of the key resource persons involved in the development of the handbook, about its significance and why people should use it.