COVID-19 and AYSRH: Program Adaptation Lessons and Stories of Resilience

On April 27, Knowledge SUCCESS hosted a webinar, “COVID-19 and Adolescent and Youth Sexual and Reproductive Health (AYSRH): Stories of Resilience and Lessons Learned from Program Adaptations.” Five speakers from around the world presented data and their experiences on the impact of COVID-19 on AYSRH outcomes, services, and programs.
Missed this session? Read the summary below or watch the recordings (in English or French) or read the transcript (in English).
Speakers

Moderator: Dr. Zayithwa Fabiano,
Witwatersrand University,
Founder, Health Access Initiative Malawi

Catherine Packer,
Senior Research Associate,
FHI 360

Dr. Astha Ramaiya,
Research Associate,
Johns Hopkins Bloomberg School of Public Health

Lara van Kouterik,
Head of Learning and Partnership Development,
Girls Not Brides

Dr. Nicola Gray,
Vice President for Europe,
International Association of Adolescent Health (IAAH)

Ahmed Ali,
Adolescent Sexual and Reproductive Health and Rights Consultant,
WHO
Catherine Packer: Impact of COVID-19 on Family Planning in Africa and Asia
Earlier this year, Knowledge SUCCESS launched the interactive experience Connecting the Dots. It explores the impact of COVID-19 on family planning in Africa and Asia. Connecting the Dots was not focused on youth, so Ms. Packer presented a new subanalysis to pull out the impact of COVID-19 on young women’s contraceptive use. This analysis used Performance Monitoring for Action data from December 2019 to January 2021. They sought to answer two questions about the pandemic’s impact on young women:
- Did pregnancy intentions or contraceptive use change as a result of COVID-19?
- Were women able to access FP services during the pandemic?
Results of the Analysis
The data show very little change in contraceptive use in women younger than 25 as well as overall. The later COVID-19 survey showed contraceptive use in Burkina Faso and Kenya was actually slightly higher than pre-pandemic levels (see graph below).
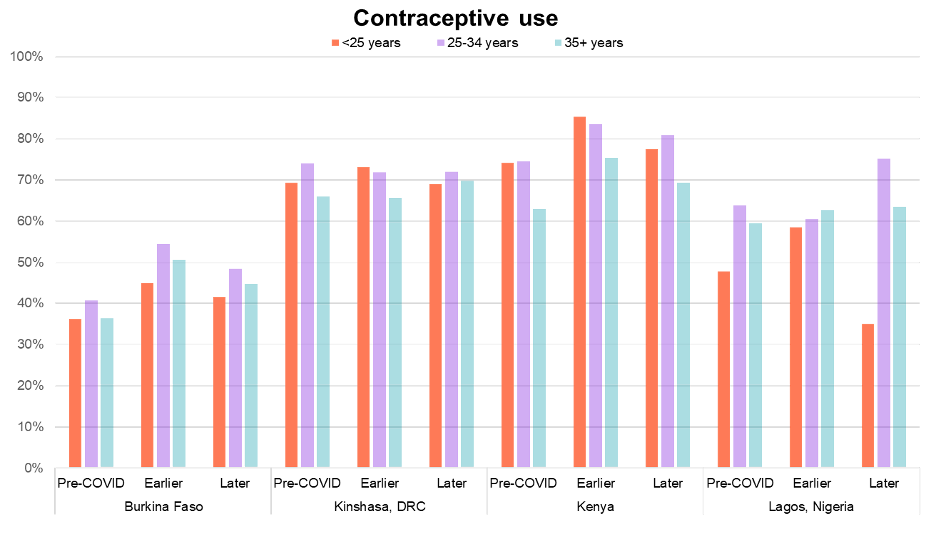
The later COVID-19 survey showed a slight increase in women switching to a less effective contraceptive method or no method at. Generally, fewer or similar percentages of younger women compared to older women switched (see graph below).
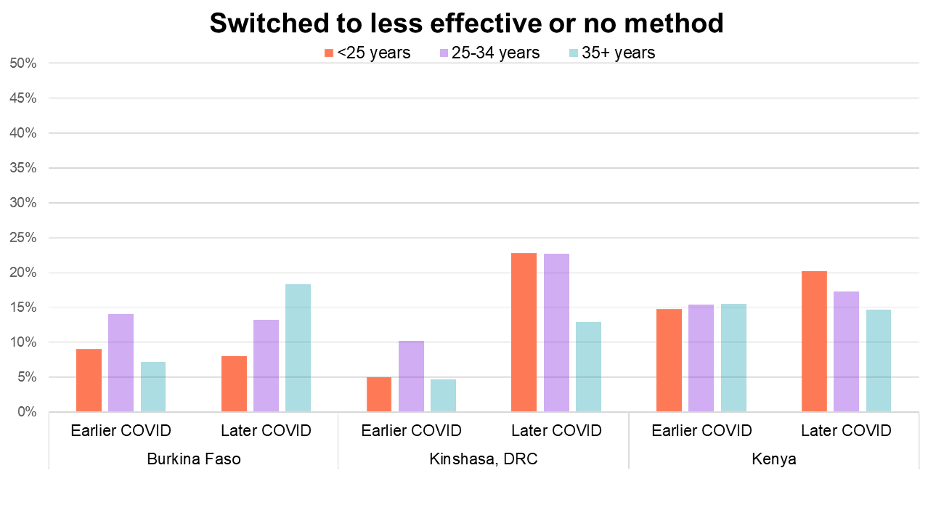
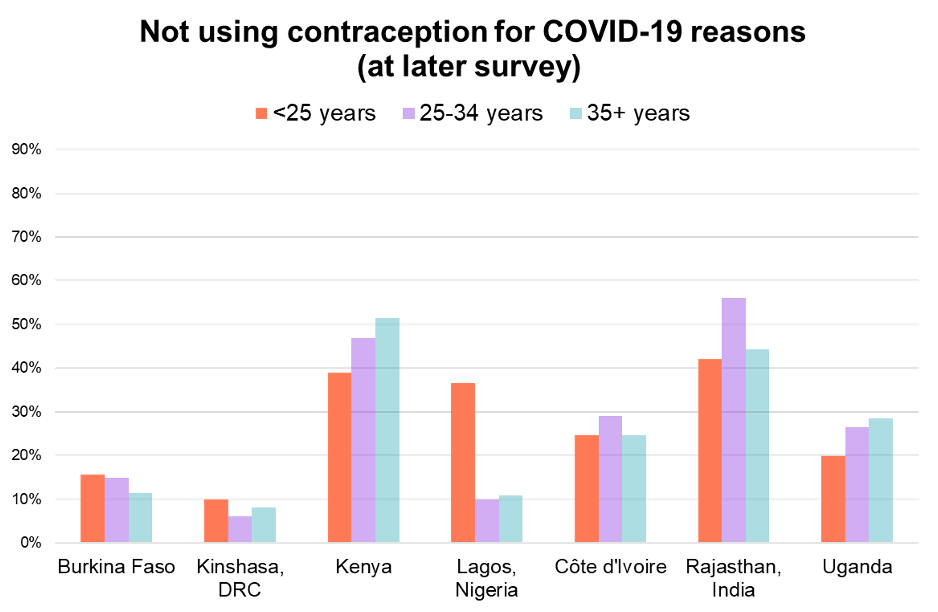
The same survey also showed that more women cited COVID-19-related reasons for contraceptive non-use. In Lagos, more younger women cited COVID-19 as a reason for non-use, but this was not the case in other settings (see graph below).
Key Takeaways
- Ms. Packer suggested that policy and program adaptations enabled women to continue contraceptive use during the pandemic. This may be the reason the impact was not as severe as originally feared.
- Depending on the indicator, there were differences in contraceptive use based on age. They were not consistent across countries or even within a country at different times. Youth data specifically could not be separated out to differentiate between adolescents (15–19) and young women (20–24). This could have revealed more insights, so we need more data to effectively analyze the impact of COVID-19 on AYSRH.
“In this analysis, it appears that COVID-19’s impacts on contraceptive use during the first year of the pandemic may not have been as severe as originally feared.”
Dr. Astha Ramaiya: Impact of the COVID-19 Pandemic on Adolescents in LMICs
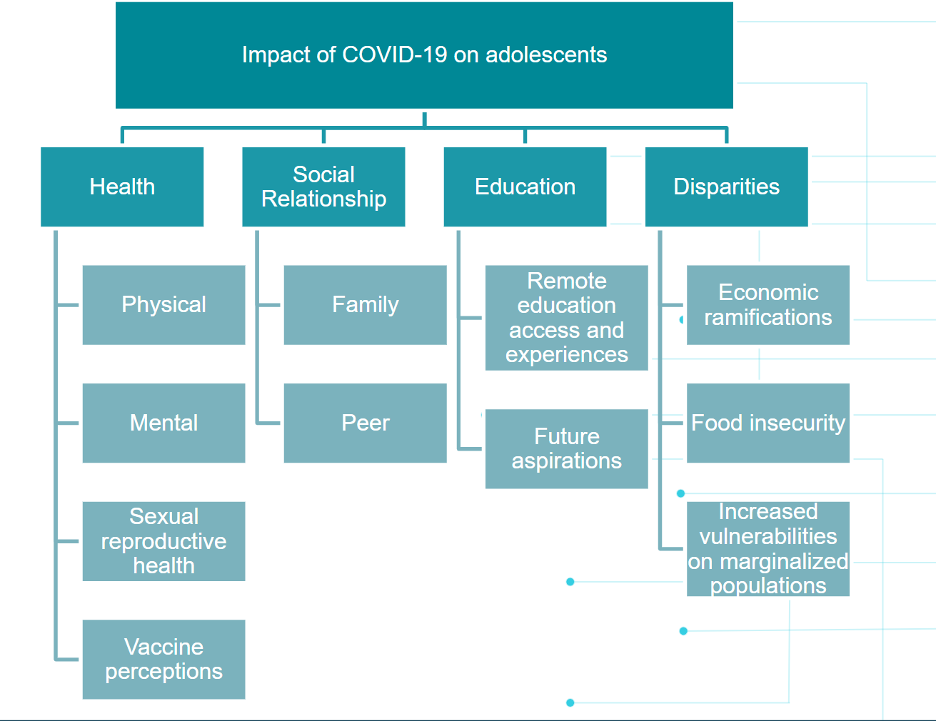
The objective of Dr. Ramaiya’s research was to map and synthesize the literature on the impact of the COVID-19 pandemic on adolescents’ health and social outcomes in low- and middle-income countries (LMICs). These outcomes were grouped as health, social relationship, education, and disparities (see chart below).
Dr. Ramaiya and her colleagues completed a rapid literature review of 90 articles to create an analysis based on a broad, sound body of evidence.
Results and Analysis
- Macro-level implications
- At the community level, Dr. Ramaiya found reports of widening gender disparities, increased vulnerabilities for special populations, and worsening economic ramifications due to the pandemic. She specifically highlighted the economic impact: 60% of young people worried about their economic future, and 80% reported a worse household economic status than before the pandemic.
- Meso-level implications
- Dr. Ramaiya discovered that young people were experiencing predominantly negative family and peer social relationships. Their education was particularly affected by COVID-19. The review noted a significant decrease in those actively engaging in learning due to factors related to remote-based education. Those factors included a lack of reliable internet connection, not enough materials or support from teachers, and more time spent engaging in paid work. This led to higher rates of early school leaving.
- Individual health implications
- The COVID-19 pandemic has widely affected health outcomes for all populations, but mental health in young people has been particularly affected. Young people reported higher proportions of depression, anxiety, stress, loneliness, and suicidal ideation.
- Dr. Ramaiya found 16 articles specifically addressing the pandemic and sexual and reproductive health (SRH). As many as 50% of adolescents could not access health care due to COVID-19 stigma, lack of access to a facility, and cost. Dr. Ramaiya mentioned the data showed that those who identified as a female especially had trouble accessing SRH care and menstrual products. In Kenya, Population Council reports girls dropped out of school at a higher rate due to unintended pregnancy.
Key Takeaways
- Dr. Ramaiya highlights the need to respond to adolescent mental health needs with evidence-based approaches and parental support. Widening economic disparities have affected marginalized adolescents who are already at risk. Programs must pay attention to these adolescents and the factors that contribute to their marginalization.
- Pandemic-related school closures led to early school leaving among adolescents. This reflects “the importance of keeping schools open, tailoring education to the needs of children, and continuing education for older adolescents who have started work.”
- There must be an effort to reduce COVID-19 stigma to ensure continuity of care, provide individualized care to vulnerable populations, and distribute menstrual products.
Lara van Kouterik, The Impact of COVID-19 on Child Marriage and Adolescent Girls
Ms. Van Kouterik began her presentation by exploring the definition of child marriage and how many girls around the world were married before age 18.
What is child marriage?
- Child marriage is any formal marriage or informal union in which one of the parties is under the age of 18.
- Worldwide, nineteen percent of girls marry before 18.
COVID-19 Impact on Child Marriage
Ms. Van Kouterik shared that COVID-19 could impact progress toward eliminating child marriage. UNICEF projects that an additional 10 million girls could enter into child marriage by 2030 due to school closures, increased rates of adolescent pregnancy, disruption in SRH care, economic shocks, and the death of parents.
Child marriage data is collected by looking at women aged 20–24 and identifying at what age they were married. This means that it is too soon to tell what kind of impact COVID-19 has had on child marriage. In order to mitigate that impact, Girls not Brides recommends ensuring access to health care and education and offset the economic shocks of the pandemic.
Regional Examples

Girls Not Brides policy brief cover.
West and Central Africa
- Girls not Brides published a policy brief with Plan International. It includes observations from members on the ground in West and Central Africa. They have found an increase in rape and adolescent pregnancy, which leads to child marriage. They also report that it is difficult to access SRH care, including postnatal care for new mothers.
 Mexico
Mexico
- In Mexico, Girls not Brides members found an increase in domestic violence calls and recorded instances of domestic violence. There were fewer abortions recorded in 2020 than 2019, likely due to women and girls not accessing health services due to the pandemic.
 India
India
- Girls not Brides members in India wrote that 89% of families reported a negative impact on their household finances due to the pandemic. Girls especially felt this change, as 25% reported feeling depressed or worried about their future opportunities. A similar percentage of girls were unable to access distance-learning materials, and their parents began to lose interest in their daughters’ educations.
Key Takeaways
- Programs must scale investment in girls’ education, SRH care, and psychosocial support. Ms. van Kouterik highlighted the essentialness of SRH care and service in times of crisis.
- Emergency-response programs should prioritize the needs of adolescent girls.
- Community-based civil society organizations (CSOs) are already working directly with adolescent girls, so these organizations need support and funding.
To learn more about the impact of COVID-19 on child marriage, head to the Girls Not Brides learning hub. Briefs are available in English, French, Spanish, Arabic, Bangla, and Portuguese.
Dr. Nicola Gray: Reflections from the IAAH Community on ASRH and COVID-19 Pandemic
Dr. Gray began her presentation with a short introduction to International Association for Adolescent Health (IAAH), a non-government organization working to improve adolescent health across the globe. In response to the COVID-19 pandemic, IAAH released a statement on protecting adolescent health during this public health emergency. Dr. Gray highlighted the projections that millions of additional child marriages and unintended pregnancies may occur as a result of the pandemic (as Ms. Packer and Ms. van Kouterik discussed earlier in the session). IAAH included recommendations on how to sustain and expand efforts to reach adolescents. Dr. Gray detailed examples from three different kinds of interventions: legislative, telehealth, and service delivery.
Legislative
In Malaysia, the government passed laws to protect adolescents by increasing the age for statutory rape from 12 to 16 years old. It also prohibited and penalized child marriage. Due to pandemic school closures and economic hardships, many adolescents were at risk of sexual violence or child marriage. This kind of legislation is a “pillar to protect ASRH.”
Telehealth Intervention
In the United Kingdom, a digital health service, Brook, launched its “digital front door” service to reach adolescents seeking SRH care through telehealth. There are a variety of challenges regarding digital health, including:
- The loss of face-to-face connection.
- A reluctance to share personal information.
- A need for clinical staff to identify those at risk.
The safeguarding of adolescents seeking care is essential to the operation of any intervention, especially digital health. In order to ensure the safety of its patients, Brook encourages those at risk to disclose it through the app. It trains staff on how to identify patients who may be at risk (those using alcohol or drugs before sex, engaging in sex with an older partner, feeling generally low or depressed).
Service Delivery Intervention
Due to COVID-19’s disruption of health service delivery in Nigeria, a network of health workers decided to adapt their services to reach adolescent girls. Adolescents 360 (A360) saw its weekly service decrease from 2,000+ pre-pandemic to 250+ in April 2020. To make sure its counselors were providing the necessary care to its patients, A360 conducted virtual trainings to provide counselors with up-to-date COVID-19 information. It also instituted a process to integrate COVID-19 into its current work. This allowed the counselors to meet face to face with their patients in their communities. There they provided SRH and COVID-19 information while implementing safety measures to mitigate the spread of COVID-19. The counselors were able to then refer patients to A360 hubs for necessary follow-ups by phone or text.
Key Takeaways
- Empower those who serve and work with adolescents to ensure they can identify and prioritize those at-risk.
- Obtain accurate SRH data and monitor the situation.
- Harness digital technology.
- Retain human, face-to-face contact.
Dr. Ahmed Ali: Lessons Learned from Adaptations to Organizations’ Responses to SRH Needs of Adolescents in the Context of the COVID-19 Crisis
Mr. Ali detailed lessons from a WHO report on ASRH care in the context of COVID-19. It detailed case studies on the work of 36 organizations from 16 countries. It was apparent that it was up to local and international organizations to keep the focus on AYSRH care, as many governments turned their sole attention to the economic burden of the pandemic.
Research Question
How did organizations adapt their responses to the SRH needs of adolescents during the COVID-19 pandemic? The WHO posted an open call to submit case studies. The case studies represented a focus on SRH services, such as:
- Contraceptive information and services.
- HIV care.
- Menstrual health information and products.
The studies mostly targeted adolescent girls and vulnerable adolescent populations such as those living with HIV, LGBTQ+ adolescents, and those living in remote areas.
Research Findings
- The service adaptations were mostly digital or remote-based. The most common adaptations were the use of social media, radio and TV, telehealth, phone consultations, and e-pharmacies. Remote adaptations mitigate the risk of COVID-19 transmission. They also respond to the gap in SRH services from COVID-19 disruption and can reach the most vulnerable populations.
- Example adaptation
- In Uganda, UNFPA partnered with SafeBoda, a motorcycle taxi app, to create an e-pharmacy. Anyone, including adolescents, could order free-of-charge reproductive health commodities through this app. The customer service team was trained specifically on how to respond to ASRH concerns and questions. They onboarded 10 pharmacies to the app with the help of a variety of partners.
- Implications for action and follow-up
- Adaptations could be used as a complement or substitute for traditional pre-COVID-19 programming. It was too soon for most studies to include proper evaluation data, so there is a need for more data on effectiveness. The WHO is planning a second phase of case study development. After 18–24 months, it wants to identify whether organizations are still using them and the results of their evaluation.
Moderated Discussion and Conclusion
Suicidal Ideation in Adolescents
Can you elaborate on suicidal ideation in adolescents?
Dr. Ramaiya: Rates of suicidal ideation and attempts ranged from 10% to 36%. Suicidal ideation was outlined in one study in China. It took two groups of adolescents: one who were “left behind” children and categorized as marginalized and then another group were not “left behind” and categorized as non-marginalized. Suicidal ideation was found to be 36% among these adolescents. For non-marginalized adolescents, factors associated with suicidal ideation included low parental education and higher anxiety and depression symptoms. For marginalized adolescents, the risk factors included being female, lower parental education, a perceived worse family economic status, and anxiety and depression symptoms.
PMA Findings
Can you offer potential reasoning why the PMA data indicating a minimal drop in contraceptive use among young women reconciles with the literature indicating increased rates of adolescent pregnancy and child, early, and forced marriage or union (CEFMU), as offered by the other presenters? Do these PMA findings align with other national/global data collection findings?
Ms. Packer: The denominator for the PMA indicator was women at risk of unintended pregnancy. This is defined as non-pregnant, non-infertile, married, or partnered women who did not want to have a child in the next year. Fewer adolescents aged 15–19 would fit this definition. We had similar findings to a recent FP2030 report. This data showed higher than expected contraceptive use in four countries and a slight decrease in two countries but overall not much change. Guttmacher data from March 2020 to December 2020 showed very little decline in adolescent contraceptive use. For Uganda, it actually increased from pre-pandemic levels. Available data are still limited, but consistently indicate that the disruptions have had less impact on SRH than initially expected. But it still may be too soon to see these impacts reflected in the data, so we have to wait a bit longer and review other data sources to understand the impact.
Crisis and Emergency Preparedness Recommendations
What are two recommendations for immediate action to mitigate crises, and also two recommendations that policymakers and program implementers should take note of, especially with regard to emergency preparedness and response?
- Ms. Packer
- Take a moment to celebrate the success that programs have had in continuing to provide critical contraceptive services.
- Webinars and case study reports can help us share, have access to, and learn from these successful program adaptations.
- We should proactively design data and collection tools to be able to analyze youth populations and capture diverse youth experiences.
- We must remember that health and education are inextricably linked. We should also look at data to show the impact of mental health on contraceptive use among youth.
- Dr. Ramaiya
- Pandemic-related economic ramifications have been adverse for the most marginalized adolescents. There is a link between the macro-, meso-, and micro-level impacts—interventions can not happen in a silo, focusing on just individualized needs.
- We need to recognize the fact that the pandemic has exacerbated the marginalization of those groups who were already marginalized, including those who are girls and from a lower socioeconomic status. We need to reduce these inequities in the future.
- Ms. van Kouterik
- Two immediate actions:
- It is essential for girls to return to school. We must guarantee 13 years of school for every child.
- The COVID-19 crisis is affecting those most at risk of child marriage. We must really look at the intersectional oppressions that girls face and prioritize the rights and needs of these girls, especially in times of crisis.
- Long-term recommendations:
- What is really important is that policymakers look at upholding human rights in times of crisis. That means prioritizing the needs of girls, including the continuation of access to essential care, SRHR care, and education, but also really consulting girls and women during the full cycle of emergency preparedness, risk, mitigation, and response.
- We must make sure community-based organizations are well-funded and have the resources they need to continue their work. They are the ones providing services, education, and support to girls, and their work is essential.
- Two immediate actions:
- Dr. Gray
- Immediate actions:
- Empowering and informing local health workers is essential to make sure no woman or girl is cut off from services, especially those living in refugee camps or in conflict zones.
- We should think carefully about the design and framework of telehealth services. Many are convinced these interventions are the “future,” but they must be cognizant of consent, confidentiality, and safeguarding when designing and implementing these tools.
- Long-term recommendations:
- Engaging and involving parents is important, as young girls are obtaining services with their parents, using their parents’ phones, and receiving their parents’ guidance.
- There should be a deeper collaboration between health workers and schools. We can extend the reach to younger adolescents by providing care via school.
- Immediate actions:
- Mr. Ali
- Immediate actions:
- The sharing of lessons learned can help stakeholders mitigate COVID-19 disruptions in SRH care, especially in regard to reaching the most vulnerable adolescents.
- Collecting data is essential in order to learn more about the long-term effect of these disruptions and/or adaptations due to COVID-19.
- Long-term recommendations:
- We must enable better and more efficient platforms for stakeholders to advocate to their governments to allow for consensus on ASRH programming.
- We should develop clear and concise messaging with stakeholders around ASRH based on our data collection to ensure progress is not reversed as a result of the COVID-19 pandemic.
- Immediate actions:




