Family Planning and Reproductive Health Access and Utilization in East Africa

From June to August 2022, 38 family planning and reproductive health (FP/RH) workforce members from Ethiopia, Kenya, Malawi, Nigeria, Rwanda, Tanzania, and Uganda came together during the 2022 East Africa Learning Circles cohort. Through structured group dialogues over four sessions, they shared and learned from each other’s practical experiences, on what works and what doesn’t in improving FP/RH access and use.
CONTEXT
Expanding access to contraception and satisfying the need for family planning are essential elements for achieving universal access to reproductive healthcare services, as called for in the 2030 Agenda for Sustainable Development.
According to the World Health Organization (WHO), the number of women who want to use family planning has increased markedly over the past two decades, from 900 million in 2000 to nearly 1.1 billion in 2020. Consequently, the number of women using a modern contraceptive method increased from 663 million to 851 million, and the contraceptive prevalence rate increased from 47.7% to 49.0%. The UN projects that an additional 70 million women will be using modern contraception by 2030.
The proportion of women of reproductive age whose need for family planning is satisfied by modern contraceptive methods (SDG indicator 3.7.1) has increased gradually in recent decades, rising from 73.6% in 2000 to 76.8% in 2020. Reasons for this slow increase include limited method choice s; insufficient access to services, particularly among young, poorer, and unmarried people; side effects (whether feared or experienced); cultural or religious opposition; poor quality of available services; user’ and provider bias against certain methods; and gender-based barriers to access.
State and non-state actors both have roles to play in ensuring that barriers to access and uptake of family planning and reproductive health (FP/RH) services are addressed. A number of different elements need to be in place for successful FP/RH programs, from strategic planning, program development, and implementation to monitoring and evaluation (M&E) and accountability.
2022 EAST AFRICA LEARNING CIRCLES COHORT
To ensure that everyone is equipped with the knowledge and best practices to address the factors hindering access to and use of FP/RH services, the Knowledge SUCCESS East Africa team hosted a Learning Circles cohort on Family Planning and Reproductive Health Access and Utilization in East Africa. This topic was identified as a regional priority according to surveys and interviews among FP/RH professionals and organizations based in East Africa.
The weekly Learning Circles sessions and discussions were anchored by the FP2030 Rights-Based FP Program Framework, which depicts essential elements that should be in place at various levels in the healthcare system, including empowered and satisfied clients, quality information and services, an enabling legal and policy environment, and supportive culture and community.
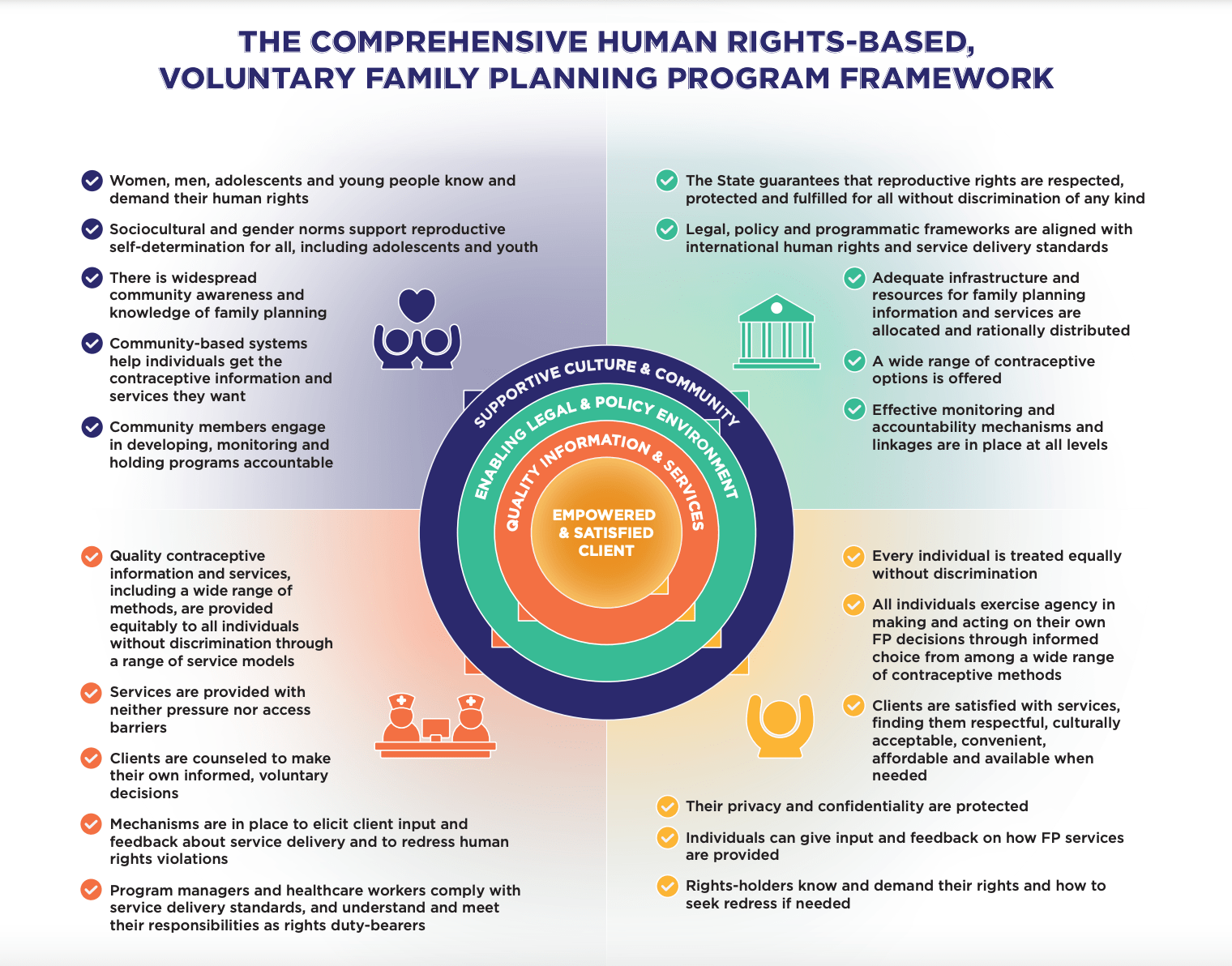
The Learning Circles cohort participants also considered the 10 human rights-related principles and standards pertaining to contraceptive information and services upon which the framework is based. These principles, agreed on by WHO, UNFPA, FP2030, and others, include:
- Availability
- Accessibility
- Acceptability
- Quality
- Non-discrimination and equality
- Informed decision-making
- Privacy and confidentiality
- Participation
- Accountability
- Agency/autonomy/empowerment
KEY INSIGHTS
Success Factors
Through small group discussions, cohort participants used Google Jamboard to brainstorm a wide range of ideas around successful strategies for improving FP/RH access and utilization.
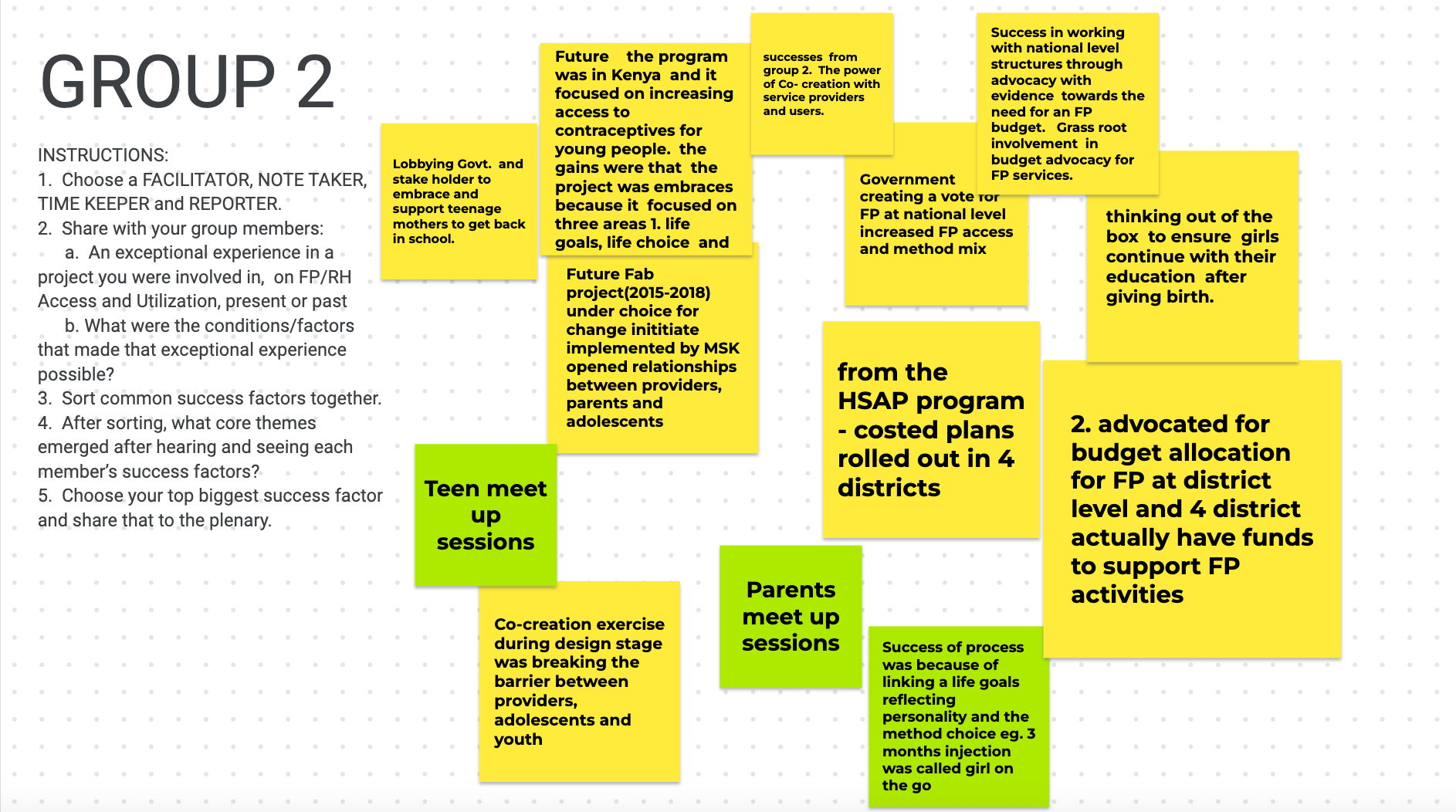
They then grouped their top success factors to align with the key elements of the FP2030 framework:
- Quality information and services: Continuously train and mentor service providers to avoid method bias, ensure availability of a wide range of method choices, improve client information sharing and counseling
- Advocacy and resource mobilization: Advocate for FP budget allocation and spending, develop of Costed Implementation Plans, ensure resources to buy commodities
- Stakeholder engagement: Engage stakeholders at all levels (including community/youth, government structures, and public-private sector partners) to provide ideas, promote collaboration, ensure ownership and sustainability
- Enabling environment: Establish and enforce legal and policy frameworks that facilitate access to and use of FP/RH services, as well as prioritizing data use for decision-making
- Socio-cultural factors: Address barriers to FP/RH access, promote gender norms that support FP access, create awareness and demand for FP/RH services, encourage male involvement, correct myths and misconceptions
Project management and coordination: Create and adhere to plans for implementation, research/surveys, M&E
Challenges
Using a knowledge management approach called Troika Consulting, cohort participants identified a number of challenges to FP/RH access and utilization:
- Project handovers: Lack of clarity regarding roles and responsibilities between international and Africa regional offices causes delays in capacity strengthening
- Limited FP/RH services on national health insurance schemes: Clients end up paying for services, making it difficult to achieve all visits
- Provider bias hampers integration of FP/RH services: Clients sometimes opt to use oral contraceptive pills instead of considering other available methods due to provider bias.
- Health facilities do not have specific youth services. Where FP services are available for adolescents, they are often provided in Care and Treatment Centers—which often cater to women who have given birth, excluding not nulliparous girls and women. When adolescent and youth sexual and reproductive health (AYSRH) is not a priority for policymakers and implementers, adolescents face age-related stigma when trying to access FP.
- Poor consultations with key stakeholders can lead to poor health outcomes. For example, in one of three counties in Kenya, poor coordination with the Ministry of Health led to delays in training health workers on the provision of adolescent-responsive services, resulting in increased rates of teenage pregnancy and gender-based violence (GBV).
- Lack of support from schools, who cite limited time during the school day, for a menstrual hygiene management project.
- Low male engagement in uptake of FP services, given the power issues and social constructs surrounding consent for FP.
- Negative social norms that prohibit young people from accessing FP despite high teenage pregnancy rates.
- Commodity security issues, especially facility stock-outs of some commodities.
- Fear of side effects of contraceptive methods and/or a lack of accurate knowledge prevents many women and adolescents from accessing FP.
TAKING ACTION
The Learning Circles series culminated in participants developing commitment statements towards improved implementation of their programs while taking into account what they had learned from each other. Participant commitments included engaging faith leaders from Christian and Islamic centers to champion FP/RH, partnering with facility-based health care providers to address youth FP/RH needs, and creating a WhatsApp group for all members of the MOH Technical Working Group for GBV and AYSRH to discuss FP-related issues.
CONCLUSION
Through Learning Circles, FP/RH workforce members from East Africa were able to grow their knowledge and strengthen their understanding of how to improve FP/RH access and utilization, network and build relationships with colleagues facing similar challenges, and generate new ideas and practical solutions for improving FP/RH program implementation. Simultaneously, they learned new knowledge management tools and techniques that they can use in their organizations to facilitate creative ways of exchanging knowledge and effective practices.
Learn more about Learning Circles and read insights from a previous sub-Saharan Africa Learning Circle on family planning programming in the context of COVID-19.
Do you want to know more about the KM tools and techniques used in Learning Circles and how to use them in your own work? Check out this resource!




